Jeremiah 2911 is no different The verse has only one meaning Jeremiah 29 is addressed to the exiles in Babylon As punishment for the sins of Judah, God was going to send the Babylonians to destroy Jerusalem and the temple and to carry away many of the people to Babylon (See Jeremiah 258–14 for one example) A SOAP ( s ubjective, o bjective, a ssessment, p lan) note is a method of documentation used specifically by healthcare providers SOAP notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick wayStandard Operating Procedures 3 variants Military, Procedure, Technology Military, Procedure, Technology 2 SOP Standard Operating Procedure Film, Military, Movie Film, Military, Movie 1

China Best Selling Toilet Soap Meaning In Hindi Skin Lightening Soap Antiseptic Soap Advanced Dermatology With C Complex Baiyun Factory And Manufacturers Baiyun
S o p meaning in english
S o p meaning in english- Personal training is evolving at an unprecedented rate, and keeping pace requires developing innovative approaches to professional skills Documenting client progress is one such skill Emerging training models require more sophisticated methods of documentation Today, trainers working with special populations often work as part This clearly means that there are quite a number of advantages and disadvantages associated with the SOAP notes Consider writing your SOAP note with the help of professional services Advantages It has already been mentioned that the main purpose of SOAP notes is to develop a uniform way of capturing patient's information in a medical facility




Bangla To English Meaning Of Soap word Com
SOP Solicitation of Proposals (various organizations) SOP Statement of Principle (various locations) SOP Standard of Perfection (American Poultry Association) SOP String of Purls (blog and shop;SOAP A chart note usually follows a very simple pattern Subjective (what the patient thinks) = S Objective (what the doctor thinks) = O Assessment (what the diagnosis is) = A Plan (what happens next) = P Not all providers dictate the "SOAP" note format; Using SOAP is good medicine Michael H Riegger, DVM, DABVP We all see these articles about what it takes to run a successful practice slick marketing, conflict management, Web pages, team training, appropriate compensation packages, etc The list is endless "You get the best out of others when you give the best of yourself"
What does SOAP mean as an abbreviation?2 Assessment This section is an analysis of the subjective and objective data In an ACADEMIC SOAP, it explains the problem both in general pathophysiological terms and in terms of what mechanism is most likely occurring in this specific patient (or herd)During your training you are expected to learn and/or review the potential mechanisms, to clearly demonstrate some of that3 popular meanings of SOAP abbreviation 1 Category Suggest to this list Alternatively search Google for SOAP
This is a howto guide for using the SOAPSTone strategy to analyze literature and speeches SOAPSTone can be used to analyze how the different parts ofO– The O stands for observation what do you see in the verses that you're reading?One of the more confusing distinctions for history students at every level is that between "primary" and "secondary" sources Primary sources are original, firsthand accounts of an event or time period




Soaps Vs Bathing Bars All You Need To Know Femina In



English To Punjabi Dictionary Meaning Of Soap In Punjabi Is ਸ ਬਣ
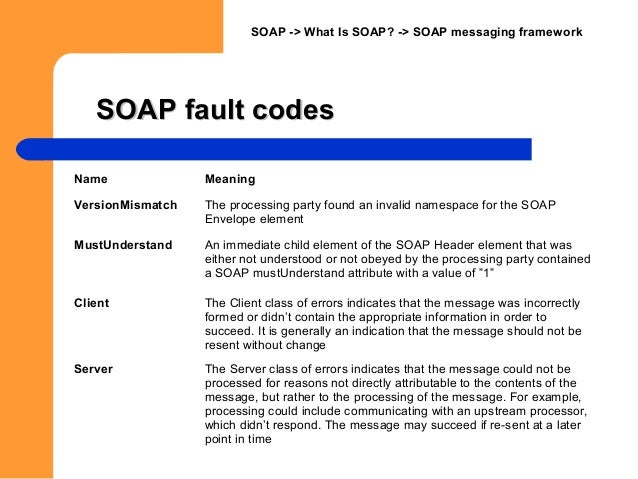
SOAP ( Simple Object Access Protocol) is a message protocol that allows distributed elements of an application to communicate SOAP can be carried over a variety of lowerlevel protocols, including the webrelated Hypertext Transfer Protocol () SOAP defines a header structure that identifies the actions that various SOAP nodes are expected to take on the2) taking possession of real property or a thing which has no known owner, with the intention of gaining ownership occupant n 1) someone living in a residence or using premises, as a tenant or owner 2) a person who takes possession of real property or a thing which has no known owner, intending to gain ownership 1 Include the patient's age, sex, and concern at the top of the note At the top of your note, write down the patient's age and sex Along with age and sex, write the patient's concern or why they came in for treatment This can help other medical professionals get an idea of diagnoses or treatments at a glance



Handwriting Text Fuzzy Logic Concept Meaning Checks For Extent Of Dirt And Grease Amount Of Soap And Water Man Holding Megaphone Stock Illustration Illustration Of Scientific Work



Handwriting Text Fuzzy Logic Concept Meaning Checks For Extent Of Dirt And Grease Amount Of Soap And Water Keyboard Blue Key Intention Create Compute Stock Photo Alamy
Best Practices The Anatomy of a SOAP Note In a previous post, we reviewed the necessity of basic best practices for SOAP notes including legibility, identification, and dated chart entries In this post, we review the proper structure and contents of a SOAP note The acronym SOAP stands for Subjective, Objective, Assessment, and Plan A SOAP note is a documentation format that massage therapists and other healthcare workers use to document client encounters SOAP is an acronym that stands for subjective, objective, assessment and plan In this post, I'll discuss An abbreviation for "Same Opposite Always Positive" used in math to simplify the process of factoring polynomials SOAP refers to whether the sign before a variable should be positive or negative



Soap Urdu Translation And Meaning The Urdu Dictionary



What Is Meaning Of Detergent
SOAP notes were first developed in 1964 as a means of providing accurate records of a patient's history, case details, prognosis, treatment and results Through the use of each of the four areas in this recordkeeping method, a social worker documents initial problems, steps taken to resolve the problem and the final results of these treatment steps'Subjective Objective Assessment Planning Implementing Evaluating Reassessing' is one option get in to view more @ The Web's largest and most authoritative acronyms and abbreviations resource SOAP notes are a way for nurses to organize information about patients SOAP stands for subjective, objective, assessment and plan Nurses make notes for each of these elements in order to provide




Olive Oil Soaps Stock Image Image Of Products Health
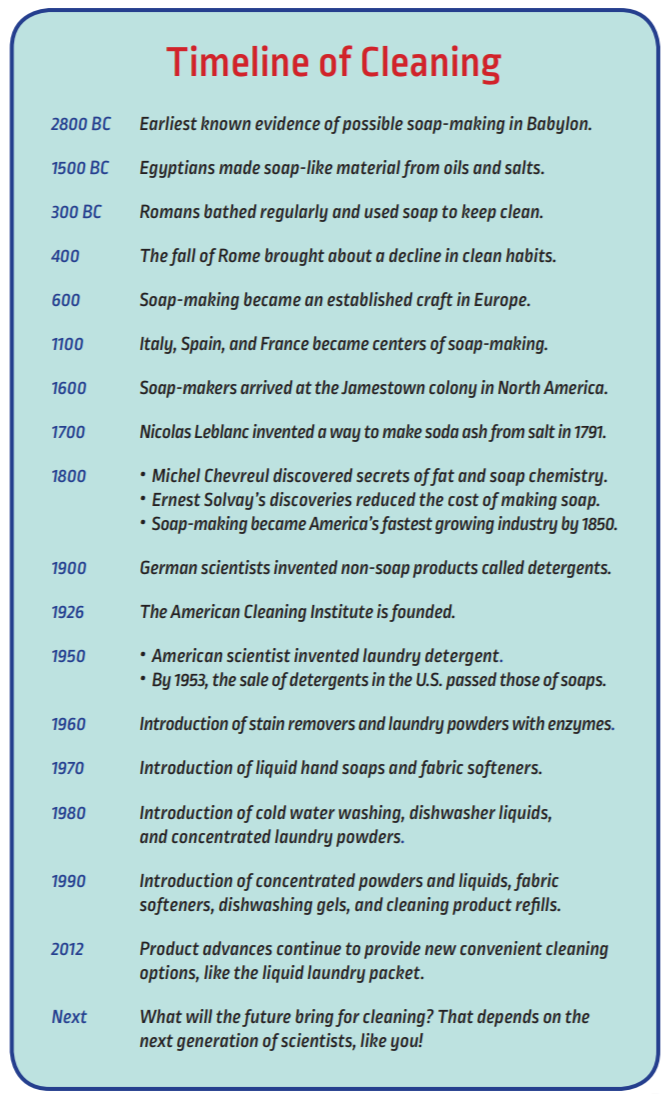



Soaps Detergents History The American Cleaning Institute Aci
SOAP Simple Object Access Protocol (XML protocol) SoaP Snakes on A Plane (movie) SOAP Standards of Academic ProgressTips for Writing Better Mental Health SOAP Notes Wed, Mar 13 – 10 PM EDT Check your email A registration confirmation has been sent to Please add webinarhost@bigmarkercom to your contacts to ensure you get aSoap definition is a cleansing and emulsifying agent made usually by action of alkali on fat or fatty acids and consisting essentially of sodium or potassium salts of




Meaning Of Web Service And Its Key Components In Soap Ui User Friendly Tech Help



Soap Emoji Meaning With Pictures From A To Z
Scale factor of size transformation In similar figures, the ratio of a distance or length in an image to the corresponding distance or length in a preimageAlso called ratio of similitude Ex When comparing the following small right triangle to its similar large right triangle, we see a scale factor of 1/2 or 05 scalene triangle A triangle with no two sides of the same length The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers The SOAP note is a way for healthcare workers to document in a structured and organized way123 The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widelyWho is the audience?




Our Soap Is Unisex Meaning Green Essentials Solutions Facebook




Soap Emoji Meaning With Pictures From A To Z
Professionals in the medical and psychological fields often use SOAP notes while working with patients or clients They are an easytounderstand process of capturing the critical points during an interaction Coaches also can make use of SOAP notes, with some adaptationsThis list contains the most common abbreviations used in the OED Click on a letter to see the abbreviations beginning with that letter Most of the words listed are onlyCategory filter Show All (39)Most Common (1)Technology (7)Government & Military (8)Science & Medicine (10)Business (4)Organizations (14)Slang / Jargon (5) Acronym Definition SOAP Simple Object Access Protocol (XML protocol) SOAP Snakes on A Plane (movie) SOAP Standards of Academic Progress SOAP Strategy on a Page SOAP Symbolic Optimizing Assembler




How To Make Soap From Scratch



1
Any compound of one or more fatty acids, or their equivalents, with an alkali Soap is detergent and used as a cleanser green soap (medicinal soap) (soft soap) a soap made from vegetable oils other than coconut oil or palm kernel oil, potassium hydroxide as an alkali, and glycerinSOAP is an acronym for easy devotions you can do on your own!Looking for the definition of SOAPIER?



Soap Opera Meaning In Urdu صابن موسیقی کے ساتھ نقل یا اداکاری English To Urdu Dictionary




Meaning Of Soap Soaps Soaped Soaping Soaps In English Chinese T Dictionary World Of Dictionary
SOAP Notes Dentistry Example 1 Chief Complaint 23 year old male presents w/ a chief complaint of "my lower left back jaw has been sore for the past few days"S History of Present Illness Pt relates history of swelling for past 3 days, asymptomatic previously Medical History Med Conditions Medications Allergies Past Sx Social Hx Asthma Albuterol None Ear Lac 09S stands for scripture, first choose one scripture from your daily reading that stood out to youO stands for observation, write out your observations about that scripture and what you learn from itA stands for application, pull out one or two application points from your observationP stands for prayer, finish your devotion bySOAP is a method of Bible reading and journaling It can be used with any daily Bible reading plan S for Scripture Open your Bible to today's reading (according to whatever plan you are following) Take time reading and allow God to speak to you When you are done, look for a verse that particularly spoke to you that day, and write it in your




China Best Selling Toilet Soap Meaning In Hindi Skin Lightening Soap Antiseptic Soap Advanced Dermatology With C Complex Baiyun Factory And Manufacturers Baiyun




The Soap Opera And Its Affect On Media Culture And Society Mr Hughes Ppt Download
SOAP notes Today, the SOAP note – an acronym for Subjective, Objective, Assessment, and Plan – is the most common method of documentation used by providers to input notes into patients' medical records They allow providers to record and share information in a universal, systematic and easytoread format Many elements of modern healthFind out what is the full meaning of SOAPIER on Abbreviationscom! SOAP stands for Scripture, Observation, Application, Prayer It's a great way to delve more deeply into your Bible reading, and record your thoughts, emotions and connections when studying scripture




Soap Meaning How To Make Soap Using Local Materials And Uses Of Soap



Meaning Of Soap In Urdu صابن Sabun Meanings Urdu Dictionary
SOAPS Interpreting Primary Source Documents What is the difference between Primary and Secondary Sources? Soapie charting is S (Subjective data) chief complaint or other information the patient or family members tell you O (Objective data) factual, measurable data, such as observable signs and symptoms, vital signs, or test values A (Assessment data) conclusions based on subjective and objective data and formulated as patientSOAPIE An acronym for a charting mnemonic S ubjective, O bjective, A ssessment, P lan, I mplementation, E valuation



Soap Subject Occasion Audience Purpose By Acronymsandslang Com




China Best Selling Toilet Soap Meaning In Hindi 150g French Perfumed Soap Premium Soap With Paper Package Baiyun Factory And Manufacturers Baiyun
Sometimes they simply state in a narrative way the same informationSOAP (an acronym for Subjective, Objective, Assessment, and Plan) is a method of documentation employed by health care providers including massage therapists to write out notes in a patient's chart A Massage Therapist's duty is to assess and treat physical dysfunction and pain of the soft tissue and joints of the body – and SOAP notesSoap definition 1 a substance used for washing the body or other things 2 a soap opera 3 to put soap on Learn more




Bangla To English Meaning Of Soap word Com




Small Meaning Handmade Soap Making Colorants Making Mica Powder Powder Pigments Soap Liquid 24 Colors Amazon In Home Kitchen
SOAPStone is an acronym for a series of questions to ask yourself when reading a piece of literature It stands for Speaker, Occasion, Audience, Purpose, Subject, and Tone It can help you understand the meanings behind works of literature, and even get you into the mind of the author This can prove very helpful on the AP® English Language= Subjective or summary statement by the client Usually, this is a direct quote The statement chosen should capture the theme of the session If adding your own explanatory information, place within brackets to make it clear that it is not a direct quoteS– The S stands for Scripture you physically write out the scriptureyou'll be amazed that what God will reveal to you just by taking the time to slow down and actually write out what you are reading!



1



Tamil Meaning Of Soap Box சவர க க ரப ப ழ வழ ப ப க க ப ப ச ச ளர ம ட
Soap opera definition 1 a series of television or radio programmes about the lives and problems of a particular group of Learn moreWhat does SOAP mean?Spectrometric Oil Analysis Program (SOAP) is a method used by aircraft operators, including several Air Forces of the World, to test the health of aircraft engines by performing frequent laboratory testing of the engine oilThe tests reveal the chemical composition of any metal particles suspended in the oil samples By comparing the results to the known chemical composition of




Carbolic Soap Wikipedia



Pdf Soap Fans Introduction By Harrington And Bielby




Wura Turmeric Saffron Bar Soap Soap Turmeric For Skin Pink Grapefruit Oil




Soap Meaning Youtube




Meaning Of Soaped Dictionary English Dictionary




Soap Dream Meaning And Symbolism



Pura Vida Goat Milk Soap



Soap Urdu Translation And Meaning The Urdu Dictionary




Soft Soap Meaning Youtube



1




Soap Opera Definition And Meaning Collins English Dictionary




Meaning Beauty Bath Sponge With Soap Inside China Manufacturer




Tumeric Saffron Handmade Vegan Soap Bar Wura Sade Baron Sade Baron Inc



Define Soap Soap Meaning Soap Examples Soap Synonyms Soap Images Soap Vernacular Soap Usage Soap Rootwords Smartvocab




What Dream About Soap Means




Soap Note Examples Occupational Therapy Quotes Clinical Social Work Speech Therapy Materials
.jpg)



Safeguard Soap Definition And More For Safeguard Soap




Here S Why You Need To Go Soap Free This Winter Sensitive Skin Care Solutions Recommended By Dermatologists




Soap Wikipedia



1




Soap Wiktionary




The Real Reason Soap Operas Are Called Soap Operas Youtube




China Manufacturer For Toilet Soap Meaning 90g Men Energy Soap New Sensation Soap With Box Baiyun Factory And Manufacturers Baiyun




The Soap Opera And Its Affect On Media Culture And Society Mr Hughes Ppt Download




China Best Selling Toilet Soap Meaning In Hindi 150g French Perfumed Soap Premium Soap With Paper Package Baiyun Factory And Manufacturers Baiyun




Toilet Soap Vs Bathing Soap Total Fatty Matter Youtube




Handmade Olive Oil Soaps With An Inscription In Greek Language Meaning Pure Olive Oil Soap Together With A Natural Sea Sponge And A Small Branch Of Stock Photo Alamy



Soap Subjective Objective Action And Plan Of Treatment By Acronymsandslang Com
/a-bar-of-white-soap-with-soap-suds-on-it-77937370-5915b4ed3df78c7a8c566360.jpg)



Saponification Definition And Reaction



What Does S O A P Mean Definition Of S O A P S O A P Stands For Subjective Objective Assessment Plan By Acronymsandslang Com




Pin On Alo Goods Soaps




Soap Dream Meaning And Symbolism




The Soap Opera And Its Affect On Media Culture And Society Mr Hughes Ppt Download




China Manufacturer For Toilet Soap Meaning 90g Men Energy Soap New Sensation Soap With Box Baiyun Factory And Manufacturers Baiyun




S O A P What Does Soap Mean In Miscellaneous




Feng Shui Wood Castile Soap




Soap Meaning Of Soap In Longman Dictionary Of Contemporary English Ldoce




Meaning Beauty Bath Sponge With Soap Inside China Manufacturer




What Does It Mean To Change An Awl For Soap




Meaning Of Soap Dictionary English Dictionary




China Best Selling Toilet Soap Meaning In Hindi Skin Lightening Soap Antiseptic Soap Advanced Dermatology With C Complex Baiyun Factory And Manufacturers Baiyun




Learn Pakistan Soap Dish Meaning




Meaning And Origin Of The Phrase Not To Know From A Bar Of Soap Word Histories




Soap Meaning Of Soap Youtube




Cut Soap For Me Slang Meaning Comedy Videos Lyrics By Thecuteabiola Nairaflaver




Synonyms For Soft Soap Thesaurus Net




Nigerians Reacts After A White Man Asked What Cut Soap For Me Means See Reactions




Soap Dish Definition And Meaning Collins English Dictionary



Soap



Soap Detergent Che Nur Nadira




Soap Definition And Meaning With Pictures Picture Dictionary Books




Why You Should Pamper Yourself With Artisan Soap Sheknows




What Does Soap Mean Soap Definitions Abbreviation Finder




Soap Meaning In The Cambridge English Dictionary




Meaning Of Soap Maker In English Russian Dictionary World Of Dictionary




Must Read The Real Meaning Of Cut Soap For Me De9jaspirit




Mango Papaya Soap Tropical Shave Shampoo Soap Round Soap Etsy In 21 Papaya Soap Glycerin Soap Soap




Soap Vs Rest Apis Which Is Right For You Soapui




Soap




Soap Definition And Meaning Collins English Dictionary




Soap Web Services Tutorial What Is Soap Protocol Example




Nila Ayurvedic Soap Made Of Pyary Soap Singapore Facebook




China Best Selling Toilet Soap Meaning In Hindi 150g French Perfumed Soap Premium Soap With Paper Package Baiyun Factory And Manufacturers Baiyun




Soap And Detergent Chemistry Uses Properties Facts Britannica




College Ruled Or Wide Ruled Notebook Paper Soap Bars At Make Meaning Paper Soap Make Meaning Ruled Notebook




Amazon In Buy Never Ending Stories American Soap Operas And The Cultural Production Of Meaning Crossroads Studies In American Culture Book Online At Low Prices In India Never Ending Stories American Soap Operas



Carbolic Soap Meaning Youtube




Colorful Float Soap Is Inspired By Art Soap Packaging Design Soap Packaging Soap




Soap Dream Meaning Top 19 Dreams About Soap Dream Meaning Net




Meaning Beauty Bath Sponge With Soap Inside China Manufacturer




Soap Meaning In Urdu With 1 Definitions And Sentences




Meaning Beauty Bath Sponge With Soap Inside China Manufacturer




Castile Soap Meaning In Tamil




Soap A Poem Sihowa Publishing




Handwriting Text Fuzzy Logic Concept Meaning Checks For Extent Of Dirt And Grease Amount Of Soap And Water Man Holding Megaphone Stock Illustration Illustration Of Colors Presentation




Soap Meaning In Hindi Soap Ka Kya Matlab Hota Hai Daily Use English Words Youtube




Make Meaning Our At Home Soap Making Creativity Kits Are Now For Sale On Amazon With Prime Shipping Choose From 6 Different Themes For Cupcake And Bar Soap Sets Shop Now Http Www Amazon Com Shops Make Meaning




Soap Notes The St John S Pa Program Survival Guide



No comments:
Post a Comment